What is Chloramphenicol?
Chloramphenicol is a prototypical broad-spectrum antibiotic. It is a bacteriostatic made of Streptomyces venezuelae by David Gottlieb and became available for clinical application in 1949. It was the first antibiotic to be manufactured synthetically on a large scale.
The pharmacokinetics and action mechanism of Chloramphenicol
Chloramphenicol is a small molecule which is extremely lipid soluble and relatively unbound to protein. It works by inhibiting protein synthesis through preventing protein chain from extending by inhibiting the peptidyl transferase activity of the bacterial ribosome. It specifically binds to A2451 and A2452 residues in the 23S rRNA of the 50S ribosomal subunit, preventing peptide bond formation. While chloramphenicol and the macrolide class of antibiotics both interact with ribosomes, chloramphenicol is not a macrolide. It directly interferes with substrate binding, whereas macrolides sterically block the progression of the growing peptide.
The distribution of Chloramphenicol in the body is not uniform. It is metabolized by the liver to chloramphenicol glucuronate, which is inactive, and the majority of the chloramphenicol dose is excreted by the kidneys as the inactive metabolite, chloramphenicol glucuronate. As a result, the highest concentrations are in the liver and kidney, and the lowest concentrations are in the brain and cerebrospinal fluid. When the meninges are not inflamed, the concentration achieved in brain and cerebrospinal fluid is around 30-50%, while the percentage rises to 89% when the meninges are inflamed.
Moreover, chloramphenicol increases the absorption of iron.
The medical uses of Chloramphenicol
Chloramphenicol is used for the treatment of infections caused by numerous Gram-positive and Gram-negative bacteria, including most anaerobic organisms such as Bacillus typhi, Bacillus dysenteriae, colibacillus, Bacillus influenzae, Bacterium burgeri, pneumococcus and so on.
Because of resistance and safety concerns, Chloramphenicol is no longer a first-line agent for any infection in developed nations, with the notable exception of topical treatment of bacterial conjunctivitis. However, due to its low price and easiness in manufacturing, it is widely used in developing countries.
Nevertheless, the global problem of advancing bacterial resistance to newer drugs has led to renewed interest in Chloramphenicol’s use. It is on the World Health Organization's List of Essential Medicines. This indicates that it is one of the most important medications needed in a basic health system.
Typhoid
The original indication of chloramphenicol was in the treatment of typhoid, especially when the organism is known to be sensitive. Chloramphenicol may be used as a second-line agent in the treatment of tetracycline-resistant cholera.
Brain-related infections
Chloramphenicol has a large apparent volume of distribution and penetrates effectively into all tissues of the body, including the brain. Because of that its blood-brain barrier penetration is far superior to any of the cephalosporins, chloramphenicol remains the first-choice treatment for staphylococcal brain abscesses. It is effective in treating brain abscesses owing to mixed organisms or when the causative organism is unknown.
Chloramphenicol is effective against the three main bacterial causes of meningitis: Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae. Therefore, in the developing world, the WHO recommend oily chloramphenicol as first-line for meningitis treatment. In the high-income world, chloramphenicol is still the main drug in the treatment of meningitis in patients with severe penicillin or cephalosporin allergy. General practitioners routinely carry intravenous chloramphenicol in their bags. Specifically in the U.S., Chloramphenicol is used in the initial empirical treatment of children with fever and a petechial rash.
Neonatal septicemia
Chloramphenicol is active against Enterococcus faecium as well. In virtue of this, it is considered for being used in the treatment of vancomycin-resistant enterococcus.
Ocular infections
Chloramphenicol is effective in treating ocular infections caused by a wide range of bacteria, e.g. Staphylococcus aureus, Streptococcus pneumoniae, and Escherichia coli, but not Pseudomonas aeruginosa. The topical formulation of chloramphenicol was commonly used as eye drops as first-line treatment of conjunctivitis.
The following susceptibility data represent the minimum inhibitory concentration for a few medically significant organisms.
Escherichia coli: 0.015 - 10,000 μg/ml
Staphylococcus aureus: 0.06 - >128 μg/ml
Streptococcus pneumoniae: 2 - 16 μg/ml
(Each of the above concentrations depends on the bacterial strain targeted. For instance, some strains of E. coli show spontaneous emergence of chloramphenicol resistance.)
The veterinary uses of Chloramphenicol
Currently, through the investigation of its pharmacokinetics in koalas, Chloramphenicol is considered the most useful treatment of chlamydial disease in koalas.
Recent not-yet-published research suggests that chloramphenicol can be used in frogs to prevent their widespread destruction from fungal infections. It has recently been discovered to be a life-saving cure for amphibians’ chytridiomycosis, which is a fungal disease responsible for the extinction of one-third of the 120 frog species since 1980.
Dose, drug interactions and drug antagonistic of Chloramphenicol
Plasma levels of chloramphenicol must be monitored in neonates and patients with abnormal liver function. Plasma levels should be monitored in all children under the age of four, the elderly, and patients with renal failure. Because efficacy and toxicity of chloramphenicol are associated with a maximum serum concentration, peak levels (one hour after the intravenous dose is given) should be 10-20 mcg/ml with toxicity >40 mcg/ml; trough levels (taken immediately before a dose) should be 5-10 mcg/ml.
Application of chloramphenicol simultaneously with bone marrow depressant drugs is forbidden.
Chloramphenicol is a potent inhibitor of the cytochrome P450 isoforms CYP2C19 and CYP3A4 in the liver. If both drugs are given concomitantly, inhibition of CYP2C19 will cause decreased metabolism and therefore increased levels of antidepressants, antiepileptics, proton pump inhibitors, anticoagulants, etc, and inhibition of CYP3A4 will cause increased levels of calcium channel blockers, immunosuppressant, chemotherapeutic drugs, benzodiazepines, azole antifungals, tricyclic antidepressants, macrolide antibiotics, SSRIs, statins, cardiac antiarrhythmics, antivirals, anticoagulants, PDE5 inhibitors, etc.
Bacteriostatic Chloramphenicol is antagonistic with bactericidal Cephalosporin.
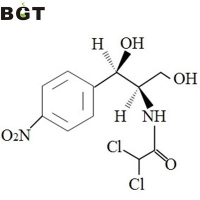
The synthesis of Chloramphenicol
The compound 2-amino-1-amino-3-phenyl-1,2-propanediol is one of the main intermediates in the synthesis of Chloramphenical. Starting from 4-nitroacetanilide, chloramphenicol can be made in high yield in a sequence of eight synthetic steps. The key step is the synthesis of a selectively protected 1,2-diol from an epoxide in an aqueous medium.